Meet Our Navigators
Every patient is different, with her own needs, questions and concerns. That’s why we take such care in personally guiding you through our entire process—from initial tests and follow-up care to your emotional support—through our navigators.
 Ida Ramos-Bendayan, RN, MSN, Clinical Nurse Navigator
Ida Ramos-Bendayan, RN, MSN, Clinical Nurse Navigator
Ida helps guide patients along the pathway to wellness after a breast cancer diagnosis. She educates and counsels patients about their diagnosis, treatment options and clinical trials available, while also referring them to the appropriate support services and community resources. As the Clinical Nurse Navigator, Ida is your central contact to help you move smoothly through the healthcare system and receive the highest standard of care in a timely manner.
Office: (845) 368-5492
Mobile: (845) 825-2902
Fax: (845) 368-5901
Ida_Ramos-Bendayan@wmchealth.org
 Cynthia Del Valle, Screening
Patient Navigator
Cynthia Del Valle, Screening
Patient Navigator
Cynthia’s role is to reach out to women who are overdue for their screening mammograms in an effort to eliminate barriers that may be preventing them from getting screened. Cynthia is your contact for whenever your patient may need extra assistance with scheduling their mammogram.
Office: (845) 368-5816
Mobile: (845) 274-3229
Fax: (845) 368-5901
Cynthia.DelValle@wmchealth.org
 Ana Paisley, Patient Navigator
Ana Paisley, Patient Navigator
Ana helps Dr. Karsif’s patients with everything from accessing resources, to appointments with specialists, follow-up care, lab work, questions, emotional support and more. As a patient navigator, Ana is your central contact to make things easier for you.
Office: (845) 357-7462
Fax: (845) 533-7200
Ana.Paisley@wmchealth.org
Hear from Our Patients

Testimonial 1: Maureen Carallo
A Star-Spangled Survivor

Maureen Corallo, a grandma and singer from Rockland County, beat breast cancer and is singing the praises of Good Samaritan Hospital.
By Debra Bresnan
I’m known as the lady who sings The Star Spangled Banner. It’s a hard song to sing, and if you start in the wrong key, it’s over,” says Maureen Corallo, 74, a grandmother of five who lives in Thiells, in the Town of Haverstraw.
Hitting the right notes in our national anthem at Little League openers, naturalization ceremonies to welcome new citizens and community events isn’t the biggest challenge in Corallo’s life though: Two years ago — just six months after her youngest son, Steve, died from glioblastoma — she was diagnosed with Her2+ breast cancer, which is often associated with a higher risk of recurrence.
Corallo first received radiation treatments for breast cancer 22 years ago at Good Samaritan Hospital, a member of the Westchester Medical Center Health Network (WMCHealth), and she returned there to undergo treatment once again. “Everyone — my doctors, the nurses and the whole team — treated me like royalty, and I felt totally confident,” she says.
In early 2016, Karen Karsif, MD, Medical Director of The Center for Breast Health at Good Samaritan Hospital, performed Corallo’s double mastectomy, and Sushil Bhardwaj, MD, Director of Good Samaritan Hospital’s Bobbi Lewis Cancer Program, administered her chemotherapy and Herceptin treatments, which she is continuing.
Comprehensive Breast Cancer Diagnosis & Treatment
“The two treatments are synergistic, and Maureen’s adjuvant regimen is a classic example of the state-of-the-art treatment available here,” explains Dr. Bhardwaj.
“I’ve had the rare opportunity to see the evolution in cancer diagnosis and treatment,” Dr. Bhardwaj says. “We’ve made tremendous strides in understanding cancer’s molecular biology and can leverage it to get rid of it or give treatments to help people live with it. The other big development is in our ability to minimize side effects, such as nausea, vomiting and infections, to give patients a better quality of life. Best of all, people receive compassionate care close to home, with a full array of services and support — from diagnosis and treatment to survivorship — right here at Good Samaritan Hospital.”
“Dr. Bhardwaj would evaluate me before each treatment,” says Corallo, adding that he assessed her overall health and once sent her to an ophthalmologist and, another time, to a urologist.
Though she temporarily lost her hair and sensation for food, she suffered no major ill effects. “The fact that I never got sick or felt weak surprised me,” Corallo admits. “Actually, the hair is coming in beautifully, and the loss of taste buds allowed me to lose 30 pounds!”
Living, With Gusto
Corallo and her husband, Sal, moved to Rockland County in 1969. They raised three children and welcomed five grandchildren into their close family circle. She sang in their church choir for more than 42 years. She joined the PTA and wrote a regular column for the local paper, Haverstraw Happenings. Before retirement, she was a judge’s secretary at the Rockland County Courthouse.
Corallo is the former co-chair of the Rockland County Breast Cancer Taskforce. “We had events and made phone calls to get the word out about mammograms,” she says. “Back when I was 51, and they found my small breast cancer, it was recommended that women get a mammogram every year until they turned 50 and then every two years after that. If I had waited until I was 52 to get mine, I might not be here today. Absolutely go get an annual mammogram.”
“I feel blessed by the kindness and care I received from everyone at Good Samaritan Hospital. The chemotherapy room has eight big comfortable lounge chairs, with all your equipment and a personal TV. It’s beautiful, clean and light… a pleasant, friendly place that makes everybody feel better,” says Corallo. “If you have to have treatments, go there.”
At the suggestion of one of her nurses, Corallo now speaks with others about her experience. “I’ll let people know how good I feel and look,” she says. “It’s definitely not the end of the world; I’m looking at it as the beginning. I have a great life, and hopefully it will last a lot longer.”
Annual Mammograms Save Lives
“Every woman should have an annual mammogram, from age 40 on,” says Steven Reichard, DO, Director of Women’s Imaging at The Center for Breast Health at Good Samaritan Hospital. “The benefits of screening mammography are significant in that the mammography is the only imaging modality that has been proven to decrease mortality from breast cancer.”
There’s been a revolution in how breast cancer can now be diagnosed and that is 3D mammography or digital breast tomosynthesis (DBT). “Research and clinical trials have proven DBT is able to diagnose up to 30 percent more breast cancers than conventional digital mammography. With this new innovation we are able to view the breast by one-millimeter slices,” says Dr. Reichard. Currently, only about 30 percent of U.S. facilities use 3D because the units are expensive, and their use requires additional training for technicians.
Good Samaritan Hospital acquired a 3D mammogram in July 2016. It is also available at two other Westchester Medical Center Health Network hospitals: Westchester Medical Center and MidHudson Regional Hospital. “It’s a huge addition to our center and fulfills our desire to provide the most up-to-date imaging technology available,” says Dr. Reichard.

Testimonial 2: Stephanie Wander
A Diary of a Survivor
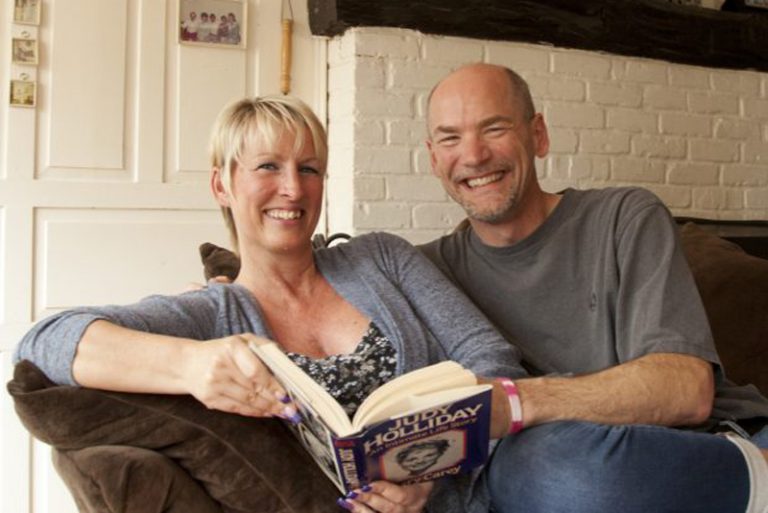
I met my current husband, Alex, in 2004, when we both worked at a luxury-car dealership. I was in the business office, and he was the parts manager. Alex likes to tell people: “It was love at first sight. I never stopped thinking about her.” We went through a lot to be together.
In 2012, we moved into a 275-year-old farmhouse in Chester and got married there on our front porch in October 2013, blending our two families into one with our four children.
The summer before our wedding, I noticed the shape of my breast was abnormal but didn’t mention it during my regular annual checkup. It became slightly worse, but I had to be ready for the wedding, finish up year-end work reports and take a business trip to Germany before I went to a March 2014 doctor’s appointment.
When my doctor advised me to see a breast specialist, I turned to Karen Karsif, MD, the Medical Director at the Center for Breast Health at Good Samaritan Hospital [a member of the Westchester Medical Center Health Network (WMCHealth)]. I chose her without hesitation because she had treated my mom for a different type of cancer. I knew if something was wrong, she was the doctor I wanted to see. After my biopsy in early April, Dr. Karsif told me I had invasive lobular carcinoma which spread to my lymph nodes. I knew something was wrong — my breast was swollen; my nipple had retracted; and my nodes were large — but it’s still unreal being told you have cancer. I was very quiet and felt numb. After a few minutes, I remember saying, “Okay, what do we have to do to get rid of this?”
Dr. Karsif recommended I undergo chemotherapy treatments first, to shrink the tumor and nodes before doing a lumpectomy or mastectomy. She said that due to the size of my tumor and the node involvement, if she had operated first, I would definitely have had a mastectomy. Most women I’ve met choose mastectomy first, then chemo. They want to get the cancer out. But I went with Dr. Karsif’s advice.
Alex went with me to all my doctor’s appointments, chemo and radiation treatments, and support-group meetings. Even though he knows I’m a very independent, strong woman, he said letting me go alone “wasn’t an option.”
I expected to lose my hair, but I was really surprised when I lost my eyebrows and eyelashes, too. Losing my nails, however, was horribly upsetting, even worse for me. I didn’t realize they would turn brown and fall off. When my hair started falling out, Alex and I shaved each other’s heads. We went through everything together.
After 16 rounds of chemo, with my tumor nearly gone, Dr. Karsif performed a lumpectomy on November 11, 2014.
I had clear margins, and she removed nine cancerous lymph nodes. The follow- up month of radiation was the thing I disliked most about all of it. For 30 days, five days a week, I had to lie in a mold with tattooed blue dots on me.
In my support group, I had what I needed: an incredible group of women. What struck me most in meetings was how different every woman is. Some told no one. Some wanted to do it alone. Others had no support. Even though I had strong support from Alex, our four children, my parents and my three sisters, my personal challenge was learning to let Alex help me.
If I had to give anyone advice, I’d say find a doctor like Dr. Karsif if you can or actually go to her. I trusted her 100 percent. Also, let people help you. Lots of women have chemo, then come home, make dinner and do the laundry. For many women, telling someone no, or saying, “I want to be alone,” or “I need to sleep,” or “I need to rest,” is difficult. But you really need to take care of you first.
Alex and I agree that breast cancer could test a marriage, but he says that any barriers we may have had are gone. He never shied away from anything because of his fear. He was strong for me.
Today, we enjoy doing everything together. We were just looking for barred owls in the woods by our lake. We like to go birding, hiking and spend time on our boat, fishing, but home is our oasis.
From the beginning, I vowed cancer wouldn’t define my life. Sometimes I’ll see a TV ad for a chemo shot and think about it, but I don’t live it every day. Now, I just look forward to making my five- year mark, my 10-year mark …
And I know I will.
Whole-Person Care
According to the American Cancer Society, breast cancer is the second- leading cause of cancer death in women, after lung cancer.
“Getting an annual mammogram is vitally important,” states Karen Karsif, MD, FACS, Medical Director at The Center for Breast Health at Good Samaritan Hospital, a member of the Westchester Medical Center Health Network (WMCHealth). “Many women think breast cancer is hereditary, but that’s true only 10 percent of the time.”
Despite recurring reports about breast cancer’s supposed causes — including underwire bras, antiperspirants, eating meat — Dr. Karsif says, “Unfortunately it’s not that simple. People ask, ‘Do I need to change my diet?’ I tell them they just need to eat healthy. You have no control over this, and that’s a huge emotional challenge.
“At Good Samaritan Hospital, we also take care of the emotional side,” says Dr. Karsif. “Our breast cancer support group is very active, and patients really help each other. We care about the whole patient, kids, family, jobs, everything.”
Dr. Karsif goes on to explain that breast cancer is especially complex because of fears of losing one’s attractiveness, femininity or identity. “I tell everyone they’ll experience PTSD; they’ll see something, and it will take them back,” she says.
“The unknown is the worst thing,” Dr. Karsif continues. “Our support group is tremendously strong and sharing. It’s a safe haven to talk about things. Many women cry because it’s the first place they feel totally comfortable. When a woman is facing mastectomy or reconstruction, group veterans, who once felt terrified themselves, offer support and are a resource for the woman.”