Receive Expert Treatment for Heartburn, GERD, Acid Reflux Disease, Esophageal Cancer and Swallowing Disorders, Close to Home
The Good Samaritan Hospital Esophageal and Reflux Center, in Suffern, NY, is a comprehensive, patient-centered initiative focused on providing solutions for patients suffering from gastroesophageal reflux disease (GERD), heartburn, esophageal cancer and other esophageal disorders.
Good Samaritan Hospital is the only hospital in Rockland and Orange counties to provide a dedicated Esophageal and Reflux Center with access to specialized physicians and surgeons. Our multidisciplinary team includes board-certified gastroenterologists, thoracic surgeons, pathologists and radiologists who work collaboratively to develop a personalized care strategy.
As healthcare becomes more complex, and treatments more sophisticated, local access to highly-skilled specialists with advanced education and training specifically in treating esophageal conditions is paramount. The Good Samaritan Hospital Esophageal and Reflux Center located in Suffern, NY provides specialist have access to state-of-the-art diagnostic tests and therapies which can help patients who have been struggling with a condition that is not getting better.
What Are the Common Symptoms of GERD?
Stephen Goodman, MD,Co-Director, Esophageal and Reflux Center, Good Samaritan Hospital, in Suffern, NY
-
A burning sensation in your chest (heartburn), usually after eating, which might be worse at night
- Chest pain
- Difficulty swallowing
- Regurgitation of food or sour liquid
- Sensation of a lump in your throat
If you have nighttime acid reflux, you might also experience:
- Chronic cough
- Laryngitis
-
New or worsening asthma
- Disrupted sleep
When Should I See a Doctor for GERD or Acid Reflux Issues?
Acid reflux is often self-diagnosed; this can be dangerous and lead to long-term issues. It is important to make an appointment with The Good Samaritan Hospital Esophageal and Reflux Center, in Suffern, NY if you experience any of the above symptoms frequently or severely or if you take over-the-counter heartburn medication twice a week.
Why Choose the Esophageal and Reflux Center at Good Samaritan Hospital?
Stephen Goodman, MD, Co-Director, Esophageal and Reflux Center, Good Samaritan Hospital, Suffern, NY
At The Good Samaritan Hospital's Esophageal and Reflux Center, in Suffern NY, you enjoy the important benefit of knowing your case is managed by a unified team directing all aspects of care and our specialists have been trained and practice at large academic medical institutions. This patient-first focus makes coordination of care between primary physicians and our specialists seamless.
- Our team of board-certified gastroenterologists, thoracic surgeons, pathologists and radiologists are focused on finding and treating the cause of your heartburn, acid reflux, esophageal cancer or other esophagus problem—not just the symptoms.
- Our physicians bring specialized skills and experience in treating GERD, acid reflux, esophageal cancer and other esophageal issues. This helps you get an accurate diagnosis and the right esophagus treatment.
- Board-certification ensures our physicians have strong training and expertise in their fields and stay up-to-date on best practices and proven treatments to solve esophageal issues.
- Our physicians have national reputations and extensive backgrounds of practice, teaching and research in esophageal care.
- The Good Samaritan Hospital Esophageal and Reflux Center, in Suffern NY, provides new technologies that increase Esophageal Cancer and GERD treatment options including, testing that makes diagnosis quicker, more accurate, and often less invasive.
April, 14, 2022
Listen to WRCR 1700 AM Radio’s “House Calls” with Dr. Stephen Goodman, Co-Director of the Esophageal and Reflux Center at Good Samaritan Hospital, a member of the Westchester Medical Center Health Network. He discusses prevention, diagnosis and treatment of GERD (gastroesophageal reflux disease), acid reflux, esophageal cancer and other esophageal disorders.
Listen to "House Calls" with Vipul Shah, MD, Co-Director, Esophageal and Reflux Center, Good Samaritan Hospital as he shares information about GERD/acid reflux and solutions.
What Are Common GERD, Acid Reflux, Heartburn and Esophageal Cancer Conditions?
Vipul Shah, MD, Co-Director, Esophageal and Reflux Center, Good Samaritan Hospital, Suffern, NY
What is Gastroesophageal Reflux (GERD)?
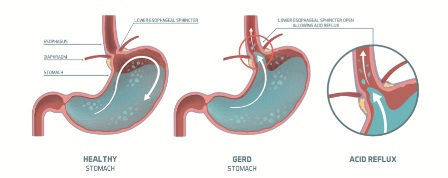
CONDITION: GERD occurs when the gastric contents of the stomach move up into the esophagus, causing heartburn, regurgitation, chest and back pain, difficulty swallowing and other symptoms related to the throat, larynx or lungs. Symptoms are often frequent or severe and lead to injury.
What are the Treatment Options for GERD or Acid Reflux?
Stephen Goodman, MD, Co-Director, Esophageal and Reflux Center, Good Samaritan Hospital, Suffern, NY
TREATMENT: Going beyond simple medical therapies, The Good Samaritan Esophageal and Reflux Center, in Suffern, NY, treats GERD that is considered refractory, meaning it is unresponsive or not fully responsive to Proton Pump Inhibitor (PPI) drugs. We also treat patients who are PPI-responsive but averse, meaning PPI drugs are effective, but the patient doesn’t want to continue taking them for various reasons. Advanced diagnostic tests are available to determine if another condition is causing the symptoms and devise customize treatment plans.
Esophageal Cancer Symptoms and Causes
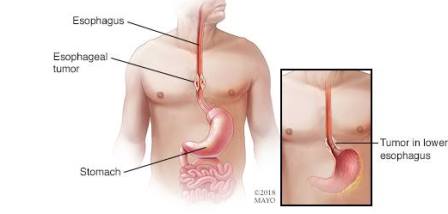
CONDITION: Esophageal cancer usually begins in the cells that line the inside of the esophagus and can occur anywhere along the esophagus. Esophageal cancer is the sixth most common cause of cancer deaths worldwide. Higher rates of esophageal cancer cases may be attributed to tobacco and alcohol use or particular nutritional habits and obesity.
Signs and symptoms of esophageal cancer include:
- Difficulty swallowing (dysphagia)
- Weight loss without trying
- Chest pain, pressure or burning
- Worsening indigestion or heartburn
- Coughing or hoarseness
- Early esophageal cancer typically causes no signs or symptoms.
When Should I See a Doctor for Esophageal Cancer?
Make an appointment at The Good Samaritan Hospital Esophageal and Reflux Center if you have any persistent signs and symptoms that worry you. If you've been diagnosed with Barrett's esophagus, a precancerous condition that increases your risk of esophageal cancer caused by chronic acid reflux, ask your doctor what signs and symptoms to watch for that may signal that your condition is worsening.
What are the Treatment Options for Esophageal Cancer?
TREATMENT: The Good Samaritan Hospital Esophageal and Reflux Center, in Suffern, NY, offers cutting-edge ablation therapies, surgery and radiation oncology treatment options.
- Esophagectomy or Esphogeal Resections
- A surgical procedure to remove part of the esophagus and then reconstruct it using some or all of another organ, usually the stomach. Esophagectomy is a common treatment for advanced esophageal cancer, and is used occasionally for Barrett's esophagus if aggressive precancerous cells are present.
- We offer laparoscopic and thoracoscopic surgical options which decrease the chance of infection, minimize pain, speed up recovery times and shorten hospital stays.
- TrueBeam™ Linear Accelerator Radiation Therapy
- The new TrueBeam™ Linear Accelerator system is an advanced radiotherapy technology for treating cancer. It targets tumors with accuracy measured in millimeters. With its power and flexibility, clinicians can develop treatments that are best suited for your individual circumstances.
What is Achalasia?
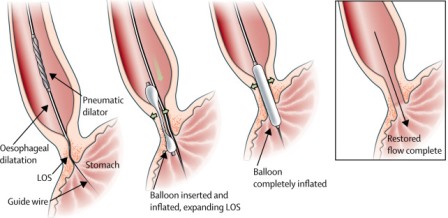
CONDITION: Achalasia is a rare disorder that occurs when nerves in the esophagus become damaged. As a result, the esophagus loses the ability to squeeze food down, and the muscular valve between the esophagus and stomach (lower esophageal sphincter) doesn't fully relax — making it difficult for food to pass into your stomach.
What are the Treatment Options for Achalasia?
TREATMENT: The Good Samaritan Esophageal and Reflux Center, in Suffern, NY, Achalasia's treatment focuses on relaxing or dilating the lower esophageal sphincter so that food and liquid can move more easily through your digestive tract. Surgical and medicinal therapy options are available.
What is Barrett's Esophagus?
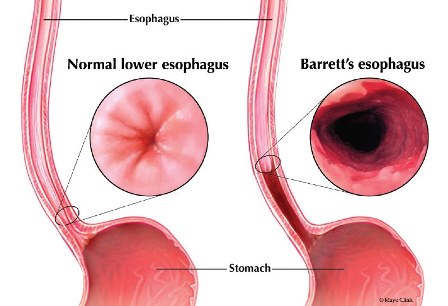
CONDITION: Barrett’s esophagus is a complication of GERD that causes erosions in the esophagus and can lead to esophageal cancer.
What are the Treatment Options for Barrett's Esophagus?
TREATMENT: Endoscopic therapies such as resection or ablation are highly successful, minimally invasive and often non-surgical treatments that can eradicate Barrett’s esophagus and prevent cancer.
What are the Most Common Esophageal Surgeries Performed at the Good Samaritan Hospital Esophageal and Reflux Center and when is Surgery the Best Option?
Mark E. Ginsburg, MD, Section Chief, Thoracic Surgery, Good Samaritan Hospital
Hiatal Hernia Signs and Symptoms
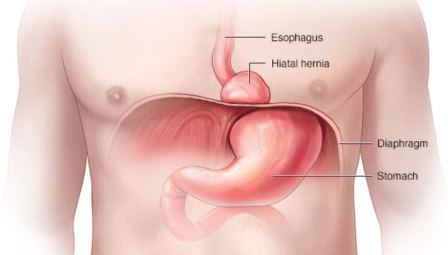
CONDITION: A hiatal hernia occurs when the upper part of your stomach bulges through the large muscle separating your abdomen and chest (diaphragm). Your diaphragm has a small opening through which your esophagus passes before connecting to your stomach. In a hiatal hernia, the stomach pushes up through that opening and into your chest.
What are the Treatment Options for Hiatal Hernia?
TREATMENT: Patients with hiatal hernias are predisposed to reflux because the top of the stomach can prolapse into the chest, bathing the esophagus with stomach acid. The Esophageal and Reflux Center offers both endoscopic and minimally invasive surgical treatments for these types of hernias.
What are Common Swallowing Disorders/Dysphagia Treatments?
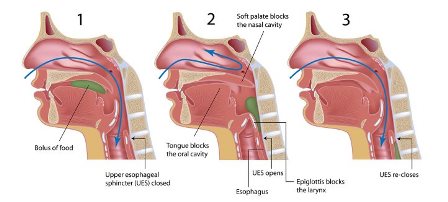
CONDITION: A swallowing disorder, known as dysphagia, may occur as a result of various medical conditions. Dysphagia is defined as problems involving the oral cavity, pharynx, esophagus, or gastroesophageal junction.
TREATMENT: Surgical and medicinal therapy options are available including esophageal dilation.
What is High-Resolution Esophageal Manometry?
Yaron D. Langman, MD, Gastroenterologist, Esophageal and Reflux Center, Good Samaritan Hospital, in Suffern, NY
High-resolution manometry (HRM) of the esophagus is a new technique that provides a more precise assessment of esophageal functions than conventional techniques.
The purpose of high-resolution esophageal manometry is to measure the pressures in your esophagus when you are resting and when you swallow. These pressures will tell us if your esophagus is working normally.
The most common uses for the test performed at The Good Samaritan Hospital's Esophageal and Reflux Center, in Suffern NY, are to:
- Diagnose esophageal motility disorders (e.g., spasms and achalasia)
- Prepare for and follow-up anti-reflux surgery
- Evaluate results of medical and surgical treatment
- Determine lower esophageal sphincter location before a 24-hour pH study
- Evaluate non-cardiac chest pain
- Evaluate non-mechanical dysphagia (difficulty swallowing)
- Evaluate rumination syndrome
Because HRM measures pressure events along the entire length of the esophagus simultaneously, the procedure time should be shorter because less catheter manipulation is required. The new HRM system is more accurate and up to 50% faster than conventional methods.
What To Expect During Your Wireless Bravo™ 48-Hour Esophageal pH Test
The Bravo™ reflux testing system is an innovative solution that measures and records the pH in your esophagus to determine if you have gastroesophageal reflux disease (GERD). The test can also be done to determine the effectiveness of medicines or surgical treatment for GERD.
During an upper endoscopy (EGD), a small capsule will be attached to the lining of your esophagus to measure and record acidity for two days. The capsule sends these measurements via radio telecommunications wirelessly to a small receiver that you will wear at waist level held by a strap over your shoulder.
You will be asked to keep a diary during the testing, including every time you eat, drink, or take medicines, and how long that lasts, when you lay down and get up and each and every time you have a symptom of heartburn, regurgitation, cough, sore throat, etc. You will return the receiver and diary when the monitoring period is over. This data will be downloaded to a computer and the results will assist our specialist in devising the most accurate course of therapy.
What To Expect During Your Esophageal 24-Hour pH/Impedance Reflux Monitoring Test
This test is performed at The Good Samaritan Hospital's Esophageal and Reflux Center, in Suffern NY, on patients who may already be on anti-reflux medication which can confuse the results of a standard pH test. Similar to the Bravo™ reflux testing, this test measures the amount of reflux (both acidic and non-acidic) in your esophagus during a 24-hour period using wireless telecommunications. It assesses whether your symptoms are correlated with the reflux or are unrelated. It takes into account that your medications will be impacting the data.
During the procedure a thin, flexible catheter with an acid-sensitive tip is put through your nose into the esophagus. The catheter is placed in separate recording spots to evaluate the flow of liquid from your stomach into your esophagus. The catheter stays in your nose for a period of 24 hours.
What Happens During Your Endoscopic Ultrasound?
Vipul Shah, MD, Co-Director, Esophageal and Reflux Center, Good Samaritan Hospital
Endoscopic ultrasound (EUS) is a minimally invasive procedure to assess digestive and lung diseases. A special endoscope uses high-frequency sound waves to produce detailed images of the lining and walls of your digestive tract and chest, nearby organs such as the pancreas and liver and lymph nodes. EUS allows your doctor to sample (biopsy) fluid and tissue from your abdomen or chest for analysis.
Endoscopic ultrasound is used to find the cause of symptoms such as abdominal or chest pain, to determine the extent of diseases in your digestive tract and lungs, and to evaluate findings from imaging tests such as a CT scan or MRI. EUS may help in the evaluation of: cancer, lymphoma, Barrett's esophagus, neuroendocrine tumors, pancreatitis and pancreatic cysts, bile duct stones and sarcoidosis.
When Would I Need a Barrx Radiofrequency Ablation and What Happens During the Procedure?
Barrx ablation is a procedure used to treat Barrett’s esophagus. With Barrett’s esophagus, the cells lining your esophagus become abnormal which can lead to the cells turning into cancer. A Barrx ablation procedure can stop them from becoming cancerous.
Barrx ablations are performed at The Good Samaritan Hospital's Esophageal and Reflux Center, in Suffern NY, during an upper endoscopy procedure. For the upper endoscopy, your doctor will use a flexible tube called a gastroscope to look at the inside of your esophagus on a monitor. Barrx ablations use radiofrequency energy (heat) to kill the abnormal cells. Killing these cells can prevent the tissue from turning into cancer. Once the abnormal cells are gone, new, healthy cells can replace them.
What is Esophageal Dilation?
The most common cause of narrowing of the esophagus is scarring of the esophagus from reflux of stomach acid occurring in patients with heartburn. Patients with a narrowed portion of the esophagus often have trouble swallowing; food feels like it is “stuck” in the chest region, causing discomfort or pain.
Esophageal dilation is a procedure that allows our doctors to dilate, or stretch, the narrowed area of your esophagus. Our experts can use various techniques for this procedure including performing the procedure as part of a sedated endoscopy. Alternatively, local anesthetic spray can be applied to the back of your throat and then a weighted dilator is passed through your mouth and into the esophagus.
Hear from Our Experts
How Common is GERD? What Could Happen if I Keep Taking Over-the-Counter Heartburn Medication and Not Seeing a Doctor?
What Are the Long-Term Effects of Using Over-the-Counter Acid Reflux Medication and Proton Pump Inhibitors (PPIs)?
Vipul Shah, MD, Co-Director, Esophageal and Reflux Center, Good Samaritan Hospital, in Suffern, NY
When a disorder of the esophagus occurs, it can cause a variety of complex problems that may affect our ability to eat, swallow, breathe or speak. Organs such as our lungs, ears or sinuses may also be affected.
For all these reasons, The Good Samaritan Hospital Esophageal and Reflux Center, in Suffern, NY, uses a multidisciplinary team approach to collaborate on each patient's case ensuring that they are thoroughly evaluated and receive the most accurate diagnosis and comprehensive treatment plans.
The Good Samaritan Hospital Esophageal and Reflux Center Leadership

Stephen Goodman, MD, Co-Director, Esophageal and Reflux Center, Good Samaritan Hospital, Suffern, NY
Board Certification
- Gastroenterology
- Internal Medicine
Specialties: General gastroenterology; advanced endoscopic interventional gastroenterology; digestive disorders, such as reflux, stomach pain, ulcers and Crohn's disease.
Education and Training
- Medical Degree: New York University School of Medicine, New York, NY
- Internship and Residency: New York-Presbyterian/Columbia University, New York, NY
- Clinical Nutrition Fellowship and Clinical Gastroenterology Fellowship: New York-Presbyterian/Columbia University, New York, NY

Vipul Shah, MD, Co-Director, Esophageal and Reflux Center, Good Samaritan Hospital, Suffern, NY
Board Certification
- Gastroenterology
- Internal Medicine
Specialties: General gastroenterology; advanced endoscopic interventional gastroenterology; pancreatic/biliary disorders and therapeutic endoscopy; digestive disorders, such as reflux, stomach pain, ulcers and Crohn's disease
Education and Training
- Medical Degree: University of Medicine and Dentistry of New Jersey (formerly Rutgers Medical College), Newark, NJ
- Internship and Residency: New York-Presbyterian/Columbia University, New York, NY
- Clinical Gastroenterology Fellowship: New York-Presbyterian/Columbia University, New York, NY
- Advanced Training in Endoscopic Ultrasonography, ERCP and Therapeutic Endoscopy: New York-Presbyterian/Columbia University, New York, NY

Mark E. Ginsburg, MD, Section Chief, Thoracic Surgery, Good Samaritan Hospital, Suffern, NY
Board Certifications
- Thoracic Surgery
- Cardiac Surgery
- Internal Medicine
Specialties: Esophageal cancer; pediatric thoracic surgery; cardiac surgery; surgery, general, lung cancer; cancer care; disorders of the diaphragm -- he is one of few surgeons in the country to perform pacing of the diaphragm.
Education and Training
- Medical Degree: Tufts University School of Medicine, Boston, MA
- General Surgery and Thoracic and Cardiovascular Residencies: University of Rochester Medical Center, Rochester, NY
Affiliations: New York-Presbyterian/Columbia University, New York-Presbyterian/Morgan Stanley Children's Hospital
Additional Esophageal and Reflux Center Physicians
GASTROENTEROLOGY

Yaron Langman, MD
Board Certification
- Gastroenterology
- Internal Medicine
Specialties: General gastroenterology; advanced endoscopic interventional gastroenterology; pancreatic/biliary disorders and therapeutic endoscopy; digestive disorders, such as reflux, stomach pain, ulcers and Crohn's disease
Education and Training
- Medical Degree: Albert Einstein College of Medicine, Bronx, NY
- Residency: Albert Einstein College of Medicine, Bronx, NY
- Clinical Gastroenterology Fellowship: Albert Einstein College of Medicine, Bronx, NY

Eric Tatar, MD
Board Certification
- Gastroenterology
- Internal Medicine
Specialties: General gastroenterology; advanced endoscopic interventional gastroenterology; pancreatic/biliary disorders and therapeutic endoscopy; digestive disorders, such as reflux, stomach pain, ulcers and Crohn's disease
Education and Training
- Medical Degree: Albert Einstein College of Medicine, Bronx, NY
- Residency: UMDNJ-Robert Wood Johnson Medical School, New Brunswick, NJ
- Clinical Gastroenterology Fellowship: UMDNJ-Robert Wood Johnson Medical School, New Brunswick, NJ
PATHOLOGY
Lori Anderson, DO, Medical Director of Good Samaritan Hospital Laboratory
Board Certification
Education and Training
- Medical Degree: Rowan University School of Osteopathic Medicine, Stratford, NJ
- Anatomic and Clinical Pathology Residency: North Shore-Long Island Jewish Health System, Manhasset, NY
- Selective Pathology Fellowship: University of Southern California - LAC and USC Medical Center, Los Angeles, CA
David Eisen, MD
Board Certification
Education and Training
- Medical Degree: University of South Florida, Tampa, FL
- Residency: New York Hospital/Cornell Medical Center, New York, NY
- Fellowship: New York Hospital/Cornell Medical Center, New York, NY
David Rubin, MD
Board Certification
Education and Training
- Medical Degree: Harvard University Medical School, Cambridge, MA
- Residency: Beth Israel Deaconess Medical Center, Boston, MA
,