Success Stories
Select a patient story below to learn more about their experience with Good Samaritan Hospital's Cardiac Care

Elizabeth and James Mooney | Two Hearts Going Strong for Valentine's Day

Thomas Donnelly | Good Samaritan Hospital Celebrates 100th Watchman Patient

Kevin Quinn | A Retired NYC Firefighter Becomes an Unlikely Heart Attack Victim

Jordan Brandeis | Active Gym Fan Surprised by Heart Condition

Michael Weisgarber |A Precise, Unexpected Diagnosis Makes A Life-Saving Difference

Denise Hurban | Arterial Bypass Grafts Got This Teacher Back in the Classroom

Linda Brancato | WATCHMAN Procedure Eliminates the Need for Blood Thinners

Kevin Meagher | TAVR Offers Minimally Invasive Heart Valve Replacement

Marcella Franks | TAVR Gets This Active Supervisor Back to Work and Fun
_____________________________________________________________________________________________________________________________
Testimonial: Elizabeth and James Mooney

Elizabeth and James Mooney, both in their 90s, have been married for almost 66 years and share four children, 11 grandchildren and seven great grandchildren. They have shared long, healthy lives and have been enjoying retirement in Florida for the past 12 years, returning to New York frequently to visit their son and daughter.
Recently, the pair started experiencing increasing fatigue and shortness of breath and underwent echocardiograms and stress tests in the care of Cary Hirsch, MD, Co-Director of the Active International Cardiovascular Institute at Good Samaritan Hospital, a member of the Westchester Medical Center Health Network.
The tests determined that both Mooneys had coronary disease and their valves had to be replaced. Dr. Hirsch recommended that they both have the TAVR (Transcatheter Aortic Valve Replacement) procedure, adding the minimally invasive procedure to the long list of everything the couple has shared together.
TAVR is a minimally invasive approach that enables the replacement of a diseased aortic valve through the use of very small incisions. It can result in less discomfort for the patient, shorter hospital stays, quicker recovery and fewer post-procedure restrictions than traditional, open-heart surgery. Their procedures were performed by cardiac surgeon, Chirag Badami, MD, and interventional cardiologists Rajiv Singh, MD and Yoram Amsalem, MD.
After her surgery in November, Mrs. Mooney said: “I got up and walked around the next day and went out for lunch!” Now, she’s attending physical therapy and they both celebrated Valentine’s Day together, although they’re anxious to get back to Florida.
“I don’t like the snow!” said Mr. Mooney.
Watch their segment on News 12
Testimonial: Thomas Donnelly
Good Samaritan Hospital Celebrates 100th Watchman Patient

L-R: Sunandan Pandya, MD, Medical Director of Echocardiography, Thomas Donnelly, Gunjan Shukla, MD, Clinical Director of Cardiac Electrophysiology, and John Zimmerman, MD, Director of Electrophysiology.
Thomas Donnelly, 67, of Sloatsburg, NY is a Dallas Cowboys fan, a retired Town of Ramapo police officer and a grandfather of four. He is also the 100th Watchman patient at Good Samaritan Hospital, a member of the Westchester Medical Center Health Network.
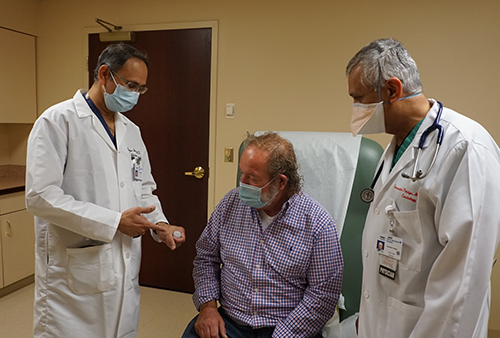 |
| Gunjan Shukla, MD, Clinical Director of Cardiac Electrophysiology (left) and Sunandan Pandya, MD, Medical Director of Echocardiography, show Thomas Donnelly the Watchman device. |
What is Watchman? It is a procedure that implants a device into a part of the heart called the left atrial appendage (LAA) and permanently closes off this part of the heart to keep blood clots from escaping. It is effective in preventing stroke in patients with atrial fibrillation, an abnormal heartbeat, who are unable to tolerate blood thinners.
Mr. Donnelly has been under the care of Cary Hirsh, MD, Co-Director of the Active International Cardiovascular Institute for many years and when he started experiencing a rapid heartbeat, Dr. Hirsch prescribed a blood thinner.
But after a few years, Mr. Donnelly was having trouble tolerating its side effects.
“I was constantly bleeding,” he said. “If my dog would jump on me, and scratch my hand with his paw, I would bleed non-stop. It was a tough medicine to deal with.”
Dr. Hirsch suggested he speak to Gunjan Shukla, MD, Director, Interventional Cardiac Electrophysiology, and John Zimmerman, MD, Director of Electrophysiology, to consider an alternative. The physicians then met with a multi-disciplinary team at Good Samaritan Hospital to verify that Mr. Donnelly was indeed a candidate for the Watchman procedure.
The medical team moved forward to perform the procedure. Sunandan Pandya, MD, Medical Director of Echocardiography, administered a special echocardiogram to guide Dr. Shukla as he implanted the Watchman device.
“Mr. Donnelly’s immediate problem was bleeding. With the Watchman, we were able to close the left atrial appendage of the heart so he doesn’t bleed anymore and at the same time, we prevent him from having a stroke,” said Dr. Shukla.
“My former boss, the Town of Ramapo Police Chief, said ‘You can go anywhere in the world with the insurance we have and we’re a half hour from Manhattan, so why would you go to Suffern, NY?’ I’m happy I did!
“You don’t have to go into New York City when you have a hospital like this right in your backyard,” he added. “Care that I was given here was second to none.
Testimonial: Kevin Quinn

A Retired NYC Firefighter Becomes an Unlikely Heart Attack Victim

This retired NYC firefighter was the picture of health — and then he had a heart attack.
By Melissa F. Pheterson
With a nor’easter predicted for Tuesday, March 14, 2017, Kevin Quinn decided to take advantage of the late-winter sun to jog outside on Monday. Quinn, 63, a retired New York City firefighter, jogged most days, rain or shine, hot or cold. But even in the calm before the storm, that run felt different.
“I was almost a mile into the run, and I felt something strange — a pressure or a pain in my chest,” he recalls. “Something stopped me. I asked myself: Was I short of breath? I was. Does my left arm hurt? It did. Normally, when I stop for aches and pains, they’re muscular; I slow down but keep running. But I knew these were symptoms of something serious.”
He was right. Two of the vessels that supply blood to his heart — the left circumflex artery and the right coronary artery — had built up enough plaque to narrow dangerously, obstructing flow. In fact, his circumflex artery (a critical branch of the left main coronary artery) had reached 100 percent occlusion, meaning no blood could pass to supply oxygen to portions of the left ventricle. His right coronary artery was 80 percent blocked. Quinn was having a heart attack, right in the middle of a West Nyack neighborhood.
Denial and Delay
Quinn didn’t have his cellphone to call 911, and while he should have rung the nearest doorbell, he admits he was still in denial at that point.
“I started to walk home very slowly, praying the whole way. When I did get home, I took a shower.” He called his sister, a nurse, to say he was thinking of driving himself to the hospital. “She said, ‘That’s the worst thing you could do,’” he recalls.
Suspecting a heart attack, she urged him to call an ambulance.
The first responders performed an electrocardiogram that confirmed the emergency. Knowing they had to bring Quinn to the most advanced level of care as quickly as possible, they took him to Good Samaritan Hospital in Suffern, a member of the Westchester Medical Center Health Network (WMCHealth). Quinn was admitted and taken straight to its cardiac catheterization lab, where Cary Hirsch, MD, FACC, Medical Director of the Active International Cardiovascular Institute at Good Samaritan Hospital, met his patient and got to work.
His team performed an angioplasty, a procedure that involves inserting a catheter through a blood vessel in Quinn’s groin, and threading it through to the heart to assess and reverse the blockage.
“We had to reopen the totally occluded artery right away,” says Dr. Hirsch. This meant inserting a stent — a mesh tube coated with medicine that slowly releases into the artery to physically open the vessel and prevent it from restenosis, restoring the flow and precious oxygen the heart muscle needs to survive.
“The doctors and nurses explained what they were doing and what I was feeling,” Quinn recalls. “I was awake during the whole procedure, and our conversation took my mind off how serious this situation could have been. It made me feel safe.”
With his patient stable and resting comfortably, Dr. Hirsch decided he would place a stent in the right coronary artery on Wednesday.
Strokes of Luck
After nightfall, a winter storm assaulted the Hudson Valley with more than two feet of snow and hazardous wind gusts. Had Quinn’s symptoms been delayed just one day — perhaps striking when he was outside, shoveling snow — the ambulance would have faced hazardous conditions while transporting him to Good Samaritan Hospital, losing critical time in the period before the heart muscle suffers irreversible damage.
On Wednesday, Dr. Hirsch performed a routine check of the left circumflex artery and found another near-complete stenosis, or blockage, slightly downstream in the artery from where Monday’s stent had been placed.
“Part of the problem with acute myocardial infarction [heart attack] angioplasty is that when you inject the artery, it’s completely occluded,” Dr. Hirsch says. “To use a driving analogy: You’re traveling at night, without headlights, and you don’t know if there’s more road ahead or not.” But now that the first stent had restored blood flow to the upper segment, lower segments had reappeared on X-rays to reveal further blockage. Dr. Hirsch had to insert another stent at the distal circumflex artery. Then the third stent was placed on the right side, as planned.
From there, Quinn recovered quickly. “I felt immediately better,” he says. “The whole blockage was slowing me down, making me tired.”
Dr. Hirsch and his team advised him to modify his diet to reduce red meat and sodium levels. A course of cardiac rehabilitation helped him return to walking and eventually running, though now he always carries a phone.
“Everyone thought I’d be the last person this would happen to,” Quinn says.
For Dr. Hirsch, this irony underscores a key aspect of heart disease.
“Among acute myocardial infarction patients, he’s an outlier: not sedentary, not diabetic or overweight, not a cigarette smoker,” Dr. Hirsch says. “Two out of three coronary arteries had major blockages, but he was running a significant amount, without symptoms. His experience shows that lifestyle is not the be-all and end-all to health and that exercise isn’t always the ‘cure’ for heart conditions. There may be genetic factors, such as hypertension, that place an individual at risk for coronary disease, despite living a healthy lifestyle.”
Quinn’s stents, combined with lowered cholesterol levels, should prevent further buildup of plaque on his arteries. Dr. Hirsch still monitors his condition and advises him on matters such as vitamins and jogging in the cold.
“I was impressed from the start with the team at Good Samaritan Hospital,” Quinn says. “From the EMTs to the nurses to Dr. Hirsch, they all pitched in to save my life.”
>> Read More Success Stories
Testimonial: Jordan Brandeis

Jordan Brandeis, 71, from New City, NY loves to stay active. He and his wife frequent their local gym five days a week, so when he was feeling some discomfort in his upper chest he did not immediately think it was a heart condition.
“I work out and I eat healthy, plus I wasn’t experiencing any of the traditional symptoms of a heart attack, like sharp pains or soreness in my arm. Thankfully, the discomfort I was feeling was strong enough that we went to the hospital on December 17, 2018,” said Brandeis.
As soon as Brandeis and his wife Libby arrived at the Emergency Department at Good Samaritan Hospital they were rushed in to see the doctor who quickly assessed the situation and called for a cardiology consult. Through an angiogram, cardiologist Andrew Shih, MD, FACC, determined that Brandeis had four complete blockages in his arteries and had suffered a heart attack. He was unable to repair the damage with stents; open heart surgery was the only option to keep the heart functioning.
“I had specifically chosen a cardiologist in Manhattan so if I ever needed heart surgery I could have it done at Lenox Hill or Columbia, and now it became clear that wasn’t an option. I had never thought I would have just minutes to make this decision,” said Brandeis.
The life-saving balloon pump Dr. Shih implanted as a temporary solution made it very dangerous to transport Brandeis. It was also a risk for him to delay the surgery anymore by traveling into the city. He and his wife immediately began researching the hospital, asking friends, family and the staff about Good Samaritan Hospital’s cardiology program.
“No one had a negative thing to say about [the cardiothoracic program] at Good Samaritan Hospital. My wife’s nephew is a doctor, and he said that the fact that we got to meet and speak to the doctors who would actually be performing the surgery was a huge plus. We would know for sure that it wasn’t someone who was learning on the job on my heart,” said Brandeis.
Cardiothoracic surgeons, Chirag Badami, MD, FACS and Cary Passik, MD, FACS both came to speak with Brandeis and his wife to explain the details of the quadruple bypass, and answer any questions to alleviate their anxiety.
“It came down to trust. I decided to stay and have the surgery at Good Samaritan Hospital because I trusted the doctors after speaking with them. They were very knowledgeable and experienced and had a great bedside manner. I felt confident in them and in my decision to stay in Rockland for my surgery,” said Brandeis.
The surgery was very successful and after five days in cardiac recovery, Brandeis was able to return home.
“We were delighted with everything at the hospital from the Emergency Department, to the pre-operation care, my doctors and nurses, the staff that took care of me in recovery. Everyone was professional and kind. They treated my wife with respect and care. The facilities and the recovery room were phenomenal and the convenience was so helpful.”
Brandeis was so impressed with his treatment, he decided to continue his follow-up care with Dr. Shih rather than travel back into Manhattan for his cardiology appointments.
“I firmly believe it was the fast action of the whole staff at Good Samaritan Hospital that saved my life – if I left the hospital I wouldn’t have made it. I realized that you can get the same level of care right here in Rockland, and you don’t need to travel. You don’t always have that choice and it is good to know life-saving care is right here.”
>> Read More Success Stories
Testimonial: Michael Weisgarber

A Precise, Unexpected Diagnosis Makes A Life-Saving Difference

Surgeons at Good Samaritan Hospital treat a dangerous heart condition called aortic dissection in the nick of time.
By David Levine
Michael Weisgarber, a special-education teacher at Orange Ulster BOCES, had just finished teaching summer school and was looking forward to his two-week vacation.
But, at his Suffern home on Sunday, August 12, 2018, he felt a pain in his chest that quickly escalated. “I could tell it was more than just heartburn,” says Weisgarber, 51. He had trouble catching his breath and experienced pain and weakness in his legs.
A neighbor drove him to Good Samaritan Hospital, a member of the Westchester Medical Center Health Network (WMCHealth), a few miles away. Quick evaluation in the Emergency Department, including a CT scan, revealed he was not having a heart attack but was instead suffering from an aortic dissection, a rare and even more life-threatening problem that requires immediate surgery.
Luckily, cardiothoracic surgeon Chirag Badami, MD, was working that Sunday. He knew how serious the situation was.
Dr. Badami called his colleague, cardiothoracic surgeon Cary Passik, MD, to come in on his day off because this complex operation required the expertise of more than one surgeon. (He also called his wife. “It was her birthday, and I told her I couldn’t take her out to dinner,” Dr. Badami says.)
An aortic dissection occurs when a tear forms in the inner layer of the aorta, the largest blood vessel in the body. As blood flows through the tear, it causes the layers of the aorta to separate, or dissect, and fill with blood. The resulting obstruction can block blood vessels and blood flow in and out of the heart, as well as cause blood leakage that can lead to shock. If this channel bursts, it can cause quick and fatal blood loss.
According to the U.S. National Library of Medicine, aortic dissection occurs in about two out of every 10,000 people. “It’s not terribly common,” Dr. Passik says. “The problem is that mortality without an emergency operation goes up about 1 percent per hour for the first 48 hours, so there is a need to get going as quickly as possible.”
Weisgarber’s situation, however, was complicated. When his aorta split, Dr. Passik explains, blood flow to his lower body was affected. This caused Weisgarber’s leg pain and weakness. If repairing the dissection did not restore blood flow to his legs, he would need more surgery.
During the procedure, his chest was opened, and his body was supported by the heart-lung machine. Utilizing a technique known as deep hypothermic circulatory arrest, Weisgarber’s body temperature was lowered to about 65°F, so that his brain and other organs could safely withstand a lack of blood flow for up to 30 minutes while the diseased, torn section of the aorta was replaced with a synthetic graft. “The patient actually has no vital signs during this portion of the operation,” Dr. Passik says. In Weisgarber’s case, it took just 14 minutes before he was back on the heart-lung machine.
Weisgarber handled the six-hour surgery without a problem, and blood flow returned to his lower extremities. He woke in the ICU that same day, was up and walking the next day and was discharged five days later.
He slowly built his stamina and strength by walking. “In a few months, I may be able to run and lift things, but not yet,” he said in October. But he can drive and hopes to return to work soon.
Risk factors for aortic dissection include uncontrolled high blood pressure, a genetic predisposition like Marfan’s disease, a preexisting aortic aneurysm, drug use that leads to high blood pressure, and heavy weightlifting, among others. None of these applied in Weisgarber’s case, and there was no family history of heart disease. So, the cause of his rupture is ultimately unknown but presumed to be genetic.
“Luckily, he came in as soon as he didn’t feel well,” Dr. Badami says, though he does advise anyone who thinks they may be having a heart attack to call 911.
“The cardiac surgical group at Good Samaritan Hospital has over 40 years of combined experience. We knew our team could handle it,” Dr. Passik says. “We have the capability to do complex procedures here. You don’t need to go down to the city. For the most part, people don’t have to look any further than this hospital for their cardiovascular care.”
Weisbarger concurs.
“How lucky for me that you can walk into a hospital on Sunday and a cardiothoracic surgeon is right there to say, ‘We have to take care of this right now,’” he says. “I got outstanding care at Good Sam. The doctors and nurses, the whole staff, were instrumental in getting me on my feet, out the door and back home.”
To learn more about cardiothoracic surgery at Good Samaritan Hospital, call 845.368.8800.
Photo By John Halpern
>> Read More Success Stories
Testimonial: Denise Hurban

Arterial Bypass Grafts Got This Teacher’s Aide Back in Her Classroom
.jpg)
The surgical team at Good Samaritan Hospital helped Denise Hurban find strength from within.
By Melissa F. Pheterson
As seen in the January/February 2020 Issue of Advancing Care
As her left arm slid off the steering wheel, Denise Hurban had one panicked thought: I don’t want to die in the car. Hurban, 50, was acutely aware of her personal and family history of heart problems. At 33, with a newborn baby, she’d learned that one of her coronary arteries had narrowed so dangerously that she needed a stent to widen it. Her younger brother had needed a similar procedure. Seared into Hurban’s memory was her father dying of a heart attack, at the wheel, at age 41.
Throughout the spring of 2019, Hurban had suffered chest pains, which she mistook for indigestion. But as a special-education teacher’s aide, she was focused on helping her students finish the school year. On June 3, her upset stomach returned as she scrubbed her bathroom floor. Reluctant to stay home and lose the day, she took antacids and began her commute from Tappan to Pearl River.
But a few minutes later, she lost her grip on the wheel. She called her daughter Bryanna, a nurse who had just finished her night shift.
“She said, ‘I think you’re having a heart attack,’” Hurban recalls.
Bryanna brought Hurban to Good Samaritan Hospital, a member of the Westchester Medical Center Health Network (WMCHealth), in Suffern. Soon after she entered the building, the numbness returned. She was seen immediately by a cardiologist, who promptly performed a cardiac catheterization and called in the surgical team.
“Denise had premature coronary artery disease and aggressive atherosclerosis — the buildup of plaque in her arteries, which is a condition that runs in her family,” says Cary Passik, MD, a cardiothoracic surgeon at Good Samaritan Hospital. Her stent had kept the disease at bay for 17 years, but the numbness and upset stomach signaled a mild heart attack.
The catheterization showed that Hurban’s left main coronary artery had narrowed. This time, however, she would require bypass surgery in which segments of blood vessels are grafted below the blockages, thus creating a new route for blood flow.
A New Take on Traditional Bypass
“While there is currently no cure for atherosclerosis, our goal is to offer surgery that will offer good health, lasting as long as possible, especially for younger patients, like Denise,” Dr. Passik explains. Traditional bypass surgeries use a combination of arteries and veins, but Dr. Passik chose to use two specific types of arteries instead: the mammary arteries (which are “almost immune to atherosclerosis”) and a radial artery, from her forearm, which also has a better chance of remaining open over the long run.
Creating a bypass with arteries instead of veins requires a longer surgery, a more meticulous technique, and because the sternum must be divided during surgery, it can take longer to heal. However, Dr. Passik, along with his partner, cardiothoracic surgeon Chirag Badami, MD, felt that Hurban was a good candidate. “This surgery is not ideal for obese or diabetic patients, or patients of advanced age,” he says.
“I have also found that bypass surgery tends to be a life-changing experience that helps patients realize they may need to change their diets, quit smoking and become more active,” he continues. “With the patient taking better care of themselves and the longevity of all arterial grafts, this procedure is as close to a cure for coronary artery disease as we have.”
Summer Vacation
With her care team working quickly, Hurban had the bypass surgery on June 5. “Dr. Passik and the nurses explained everything to my daughter and spoke to her immediately after surgery. They were thorough; they put us at ease, and their bedside manner was amazing,” she says. “I have deep respect for Dr. Passik and his team.”
Determined to return to school in September, she spent the summer recovering while trying to cultivate healthier lifestyle habits: taking nature walks, watching movies, reducing salt intake and placing chicken and vegetables in regular rotation at dinnertime.
When the first bell of the school year sounded, she was back in action — and ready to ring in a new chapter.
>> Read More Success Stories
Testimonial: Linda Brancato

.jpg)
Linda Brancato, with her husband, Stan, is happy she finally got the help she needed.
By Deborah Skolnik / Photos by John Halpern
Linda Brancato had a heart rhythm disorder but couldn’t tolerate the medicine that normally treats it. Luckily, a physician at Good Samaritan Hospital offered a minimally invasive treatment.
Having spent 21 years in the fast-paced world of retail sales, Linda Brancato didn’t think anything was amiss when she began to have spells that felt like anxiety attacks. “My heart would race, and I’d get lightheaded and dizzy,” recalls the 67-year-old Monroe resident. “I felt like I had to hold on to someone or something, because I thought I could pass out.”
Life slowed down when Brancato retired, yet her spells only grew longer. A cardiologist performed a range of tests and had her wear a heart monitor. Based on data the device had recorded, she was diagnosed with paroxysmal (or occasional) atrial fibrillation, or AFib, an irregular and often rapid heartbeat.
Blood Thinners Lead to Dangerous Bleeding
During AFib, the heart’s atria (two upper chambers), beat irregularly and out of sync with its two lower chambers. Because of this, blood clots can form in the atria and can then circulate throughout the body. Depending where they end up, these clots can cut off blood supply to organs or cause a stroke or heart attack. “I was disheartened by this news,” Brancato recalls.
She was prescribed a blood thinner to help prevent blood clots. However, the medication’s side effects required an alternative solution to prevent clots without the use of medication.
Answers at Last
She soon learned about a procedure where a device called a Watchman is implanted in the heart to help prevent clots without the use of blood-thinner medication.
She consulted with Gunjan Shukla, MD, an electrophysiologist at Good Samaritan Hospital, a member of WMCHealth. “I left his office with a smile on my face, knowing I was going to get the help I needed.”
Preparing for the Procedure
Two days before her implant, Brancato visited Sunandan Pandya, MD, a cardiologist at Good Samaritan Hospital.
“I performed a transesophageal echocardiogram, also known as a TEE, on Linda,” he says, “to look at the heart in detail.” He took images of her heart and paid particular attention to a pouch within the front of the heart’s left upper chamber, called the left atrial appendage, or LAA, where the majority of blood clots due to AFib form.
The Watchman would be implanted there, sealing it and preventing clot creation. After the TEE, which lasted about 30 minutes, Brancato went home to await her procedure.
The following day, Dr. Shukla performed the Watchman procedure (see sidebar). She stayed overnight in the hospital and was discharged the following day.
Success!
Brancato had a follow-up transesophageal echocardiogram, this time to ensure there were no leaks around the Watchman. Dr. Pandya also checked that the heart’s internal skin, called the endothelium, had grown over the device, covering it as expected. All looked well, and Brancato was cleared to discontinue blood thinners.
While she still manages her AFib with medication, Brancato is not currently symptomatic. Equally important, she no longer needs to worry about the possible side effects of blood thinners. “I have to give a shout-out to everyone I met during this process, from the door greeter at Good Samaritan to the nurses and doctors. I have such gratitude for my nurse coordinator, Suzanne Bartman, for checking in with me and visiting me and guiding me through the process,” she says. “They were all incredible.”
"Do your research on the procedure to familiarize yourself with what is ahead. Make sure you are comfortable with the doctor you choose". — Linda Brancato.
>> Read More Success Stories
Testimonial: Kevin Meagher

Kevin Meagher, 90, has been a resident of Suffern, NY, for over 50 years. His journey with Good Samaritan Hospital began in 2017, when he experienced a heart attack that caused a dangerously low heart rate and severe leaking of his mitral valve. In the ED, Meagher met cardiologist, Rajiv Singh, MD, who is a part of the Good Samaritan Hospital HeartSTAT program. Through this program he immediately underwent emergency stenting of multiple blocked arteries. The leaking of his mitral valve was successfully resolved, and he went home with a full recovery.
Meagher continued as an outpatient with Dr. Singh, with close monitoring of his coronary arteries, stents and heart valves. “I felt very confident with Dr. Singh, he was always very thorough and took the time to explain things to me,” said Meagher.
During the COVID pandemic, Meagher noticed that he experiencing shortness of breath when walking or playing golf. Dr. Singh performed an ultrasound of his heart, confirming that Meagher had a calcified aortic valve that had trouble opening, called stenosis. He recommended a valve replacement.
Fortunately for Meagher, the Transcatheter Aortic Valve Replacement (TAVR) Program at Good Samaritan Hospital had recently been introduced. TAVR is a minimally-invasive approach that enables the replacement of a diseased aortic valve through the use of very small incisions. It can result in less discomfort for the patient, shorter hospital stays, quicker recovery and fewer post-procedure restrictions than traditional, open-heart surgery. Meagher was living independently and walking freely prior to his valve symptoms, making him an excellent candidate for TAVR.
In addition to Dr. Singh, Meagher’s TAVR team included cardiothoracic surgeons, Cary Passik, MD, FACS, and Chirag Badami MD, FACS, imaging specialists, anesthesiologists, cardiac nurses and a valve nurse coordinator.
Meagher successfully underwent the TAVR procedure without complication, and was surprised how quickly he recovered. “I had the surgery on a Monday and I could not believe I was headed home on Tuesday! I was able to take a walk around the recovery room and I felt an immediate difference. I thought I would feel weaker, but I was able to get back to all of my old activities,” said Meagher.
Meagher was very impressed with the staff at Good Samaritan Hospital and would recommend the TAVR procedure to anyone experiencing the debilitating symptoms of aortic stenosis. In addition to spending time with his family, he is looking forward to getting back on the golf course this spring!
>> Read More Success Stories
Testimonial: Marcella Franks
Marcella Franks, 77, of Port Jervis, NY, likes to stay active and despite officially retiring 13 years ago, she continues to work part-time as a Production Supervisor at Kolmar Labs. Her job keeps her busy and she is always on her feet, so when she started to experience increased fatigue and shortness of breath early this fall, she went to her primary care provider and cardiologist, Walter Kaufmann, MD of the Bon Secours Medical Group. Dr. Kaufmann recommended she have an echocardiogram at Bon Secours Community Hospital and the results showed that her heart value needed replacing.
As part of the collaborative network of quality care, Dr. Kauffman referred Franks to fellow Bon Secours Medical Group cardiologist, Rajiv Singh, MD, who is part of the new Transcatheter Aortic Valve Replacement (TAVR) Program at Good Samaritan Hospital in Suffern, NY. Franks was excited to hear about the minimally invasive valve replacement solution and was impressed during her first consultation with Dr. Singh.
“Dr. Singh took the time to sit down and walk me through the entire TAVR procedure. He gave helpful examples and showed me specific images of what to expect. It was like talking to a close friend. His demeanor and expertise eliminated the fear of the unknown and made me confident I was making the right choice. Dr. Singh and the team at Good Samaritan Hospital went the extra mile and researched a custom solution that was tailored to my exact heart valve,” said Franks.
TAVR is a minimally-invasive approach that enables the replacement of a diseased aortic valve through the use of very small incisions. It can result in less discomfort for the patient, shorter hospital stays, quicker recovery and fewer post-procedure restrictions than traditional, open-heart surgery.
In addition to Dr. Singh, Franks’ TAVR team included cardiothoracic surgeons, Cary Passik, MD, FACS, and Chirag Badami MD, FACS, imaging specialists, anesthesiologists, cardiac nurses and a valve nurse coordinator.
Franks successfully underwent the TAVR procedure without complication. “I was able to go home the very next day after my TAVR. I do not believe I would have recovered as quickly or as well as I have had it not been for the positive energy of the entire Good Samaritan Hospital staff. The team is incredibly professional, compassionate and personal. Suzanne Bartman, BSN, RN, CCRN, the valve nurse coordinator, was with me every step of the way. She is a wonderful resource,” said Franks. In addition to spending time with her family, Franks is enjoying taking long walks and bike rides with friends again!
>> Read More Success Stories